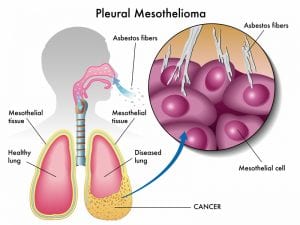
 Pleural mesothelioma is a type of cancer that develops from the thin layer of tissue that covers the lungs and chest wall. Signs and symptoms may include shortness of breath due to fluid around the lung, chest pain, cough, and fatigue. This cancer is caused by exposure to asbestos.
Pleural mesothelioma is a type of cancer that develops from the thin layer of tissue that covers the lungs and chest wall. Signs and symptoms may include shortness of breath due to fluid around the lung, chest pain, cough, and fatigue. This cancer is caused by exposure to asbestos.
It can often take around 40 years for pleural mesothelioma to begin. Imaging studies such as X-rays or CT scans may help in the diagnosis, but the disease is usually confirmed by a tissue biopsy.
Pleural mesothelioma occurs in about 2,000 people in the United States every year. Rates of pleural mesothelioma vary throughout the world and are highest in Australia and the United Kingdom. The disease occurs more often in men than women. Diagnosis typically occurs in people over the age of 60, but pleural mesothelioma has occurred in people in their twenties.
Conventional treatment may include surgery, radiation therapy, and chemotherapy (cisplatin and Alimta). According to medical studies, the median survival with conventional treatment is little more than a year.
How Do I Know If I Have Pleural Mesothelioma?
Symptoms of pleural mesothelioma are frequently confused with symptoms of other, less severe respiratory diseases. Consequently, this confusion of symptoms frequently leads to a wrong diagnosis which can delay treatment and make the battle with pleural mesothelioma even more difficult. Since the quality of life for an individual diagnosed with pleural mesothelioma can depend on early detection, it is paramount that people understand the signs and symptoms of this disease and obtain medical attention as soon as possible. Due to the difficulty in diagnosis and the confusion of symptoms, many people may ask the question, “How do I know if I have pleural mesothelioma?”
Signs and Symptoms of Pleural Mesothelioma
The signs and symptoms of pleural mesothelioma may mimic those of less severe respiratory conditions. Nevertheless, if you have a history of asbestos exposure and develop pain in the chest or lower back, shortness of breath, cough, fever, excessive sweating, fatigue, unexplained weight loss, or trouble swallowing, you should seek medical attention to investigate the possibility of pleural mesothelioma. Due to the vagueness of the symptoms, signs and symptoms alone cannot definitively tell you if you have pleural mesothelioma.
Imaging Studies for Pleural Mesothelioma
A chest x-ray is normally the initial imaging study performed on a patient who is experiencing symptoms. Although a chest x-ray is important for detecting early signs of mesothelioma, it cannot provide sufficient information to offer a definitive diagnosis. Advance imaging techniques such as CT, MRI and PET can be of greater benefit. Computed tomography (CT) scans can create a detailed 3-D image that allow tumors to be discovered easily. CT scans are approximately 90% sensitive for detecting pleural malignant mesothelioma. Magnetic resonance imaging (MRI) can also create high-resolution 3-D images than can be useful for planning a biopsy or surgical removal of the mesothelioma tumor. Positron emission tomography (PET) is excellent at identifying cancer, detecting metastasis, and distinguishing between malignant and benign diseases.
N-ERC
N-ERC/Mesothelin is a protein that may be found in the bloodstream of a patient with pleural mesothelioma. Testing for the presence of N-ERC/Mesothelin is 95% sensitive which makes it one of the most accurate blood tests available for mesothelioma.
Biopsy for Pleural Mesothelioma
Although signs, symptoms, imaging studies, and blood work may all indicate the presence of pleural mesothelioma, the only definitive way to know if you have the disease is to obtain a biopsy. The tissue that is examined during a biopsy will determine if the tumor is definitively mesothelioma or another form of cancer. In addition, a biopsy can indicate the stage of the disease and assist in determining the proper course of treatment.
Knowing the signs and symptoms of pleural mesothelioma is really the first step in knowing whether or not you have the disease. Seeking medical attention upon occurrence of symptoms can greatly enhance quality of life if you are definitively diagnosed with pleural mesothelioma. However, the answer to the question, “How do I know if I have pleural mesothelioma?” is to have a tumor biopsied.
How is Pleural Mesothelioma Diagnosed?

The road to a definitive diagnosis of pleural mesothelioma can sometimes take weeks. Pleural mesothelioma can be difficult to diagnose because the symptoms associated with this condition are non-specific. In the early stages, people with pleural mesothelioma commonly experience shortness of breath, chest pain, persistent dry cough, and unexplained weight loss. These commonly are commonly associated with other, more common, medical conditions such as coronary artery disease, chronic obstructive pulmonary disease, and influenza. Consequently, these conditions are normally ruled out before a definitive pleural mesothelioma diagnosis is obtained.
Physician Consult
The first step in a diagnosis of any medical condition is having a consultation with a physician. The physician will obtain a complete medical and occupations history. Since mesothelioma is almost always caused by exposure to asbestos, the occupation aspect of the history will be extremely important. Once the medical and occupational history has been obtained, the physician can move on to diagnostic testing.
Medical Imaging
A chest x-ray is commonly the first step to achieving a diagnosis of pleural mesothelioma. Although a chest x-ray does not provide enough information to confirm a diagnosis, it can reveal early signs of mesothelioma, such as fluid in the lungs. A computerized tomography (CT scan) can create a 3D image that allows tumors to be easily detected. Magnetic resonance imaging (MRI) can also create high-resolution 3D images which can be useful for planning a biopsy or planning a biopsy or surgical removal of the mesothelioma tumor. Positron emission tomography (PET) may also be used.
Blood Tests
N-ERC/Mesothelin is a protein that is commonly found in the bloodstream of people with mesothelioma. Testing for this protein has been proven to be 95% sensitive and is one of the most accurate blood tests available for the diagnosis of mesothelioma. Recent clinical trials have shown that testing for the HMGB1 protein, high mobility group box protein 1, can reveal a mesothelioma diagnosis. The presence of this protein may also be indicative of people who have been exposed to asbestos but have not yet developed pleural mesothelioma.
Biopsy
The only definitive method to obtain the diagnosis of pleural mesothelioma is through a biopsy. A biopsy involves the removal of cells, fluid, or a fragment of tissue for analysis. This analysis will be able to determine whether the tumor is pleural mesothelioma or another form of cancer. In addition, a biopsy can determine the stage of the disease and assist in determining the course of treatment.
Thoracoscopic Biopsy and VATS
There are various kinds of biopsies, but the most common one is a thoracoscopic biopsy. This is sometimes called open pleural biopsy and it allows doctors to see into the pleural space and remove multiple tissue samples during the same procedure. Most doctors use video-assisted thoracoscopic surgery (VATS), which uses a camera and other instruments to collect samples.
Although thoracoscopy provides the best results compared to other techniques, the procedure may not always be possible because of the tumor’s location and the patient’s state of health. Therefore, there are other types of biopsies that doctors use to diagnose mesothelioma.

Fine-Needle Aspiration
Fine-Needle Aspiration or “FNA” biopsies use a long, hollow needle to remove thousands of sample cells for testing. This procedure can access hard-to-reach areas without the need for anesthesia. According to some studies, FNA biopsies can diagnose pleural mesothelioma with an accuracy over 80%.
Thoracentesis
This procedure uses a hollow needle to remove fluid and air from the space between the pleural lining and the lungs. It can be used therapeutically to remove excess fluid that causes pain and decreases lung function, or it can also be used diagnostically to obtain fluid samples for analysis.
Thoracotomy
A thoracotomy is a kind of surgery used to access the lungs, heart, and other organs nearby. For mesothelioma patients, a segmentectomy (also called a “wedge resection”), is often the kind of thoracotomy used. During a wedge resection, a wedge-shaped piece of the lung is removed and sent to the pathology lab to be tested.
Endoscopic Biopsy
An endoscopic biopsy is a very common biopsy technique. An instrument called an endoscope is used. This tool allows the surgeon to see where he or she wants to take a sample. Forceps are usually attached to the endoscope to allow the doctor to take a small sample of the tumor.
Incisional and Excisional Biopsy
In an incisional biopsy, a small section of the tumor is removed. During an excisional biopsy, the entire tumor or lesion is removed, not just a small sample.
How Do I Choose The Best Pleural Mesothelioma Treatment?

A diagnosis of pleural mesothelioma can be devastating physically, emotionally, and financially. Advances in modern medicine have allowed for the improvement of pleural mesothelioma treatment and, although there is no definitive cure for the disease, a variety of treatment options can extend the duration and quality of life for many people with mesothelioma.
Selecting Conventional Treatments
Traditionally, there have been four major approaches to treating pleural mesothelioma. These include: surgery, radiation therapy, chemotherapy, and clinical trials. These first three approaches may be used alone, but are often combined to improve the treatment outcome.
Surgical interventions, a pneumonectomy or pleurectomy, can be performed to remove the disease. However, a pneumonectomy is considered to be a high-risk procedure and eligibility for this option depends on the overall state of health for the patient. Radiation therapy may be used alone or as a combination treatment along with surgery. Radiation therapy is focused on destroying tissue and stopping the growth of malignant cells. However, as with most treatments, a high dose of radiation can cause other health complications. Chemotherapy may be used alone or in tandem with surgery and/or radiation. The objective of chemotherapy is to destroy cancer cells and reduce tumor size. The main issue with chemotherapy is that it causes many side effects including a decrease in white blood cells that can lead to a life threatening infection. Typically, chemotherapy and radiation therapy are considered palliative treatments – they don’t cure cancer but help manage symptoms.
Clinical trials are essentially new treatments that are being tested to see how well they work. Some clinical trials use biological treatments that harness the body’s own defense mechanisms to fight tumor cells. Biological therapies may include immune therapies (sometimes called immunotherapies) that are designed to restore or enhance the body’s immune system to help it destroy cancer cells.
Selecting Alternative Treatments
People with pleural mesothelioma often consider complementary or alternative treatments while weighing their treatment options. Many traditional treatments are limited in their effectiveness and often cause side effects. Some alternative approaches such as cannabis oil, intravenous Vitamin C, Traditional Chinese Medicine, and medicinal mushrooms, have been used by mesothelioma patients. Some of these patients report that they believe these approaches have helped them. It is always best to consult your licensed healthcare professional when considering any non-FDA approved approaches.
How to Get Help for Pleural Mesothelioma

Receiving a diagnosis of pleural mesothelioma can be overwhelming. People begin to worry about many things including finances and caregivers, as well as the future of their own well-being. This fight should not be handled alone. There are a variety of support groups, medical, and legal resources that are available to help people deal with this devastating diagnosis.
Support Groups
One of the most comforting resources that someone with a definitive diagnosis of pleural mesothelioma has are support groups. Support groups allow people with mesothelioma and their caregivers to speak with others who are battling disease and seek information about how to deal with this unfortunate medical condition. Support groups are available via telephone, online, or in person so the patient can choose whatever format is most comfortable.
Medical Assistance
Once a diagnosis of malignant mesothelioma has been obtained, it is a good idea to consult with a physician who is a specialist in malignant mesothelioma. Because this is a rare disease there are only a small number of doctors with specialized knowledge and expertise in this area. It is best to get consultations with one or more of them. In addition, if conventional therapies do not provide a reasonable hope of a cure, it is a good idea to research clinical trials and alternative approaches by meeting with doctors who have expertise and experience in these areas.
Legal Assistance
Mesothelioma is caused by asbestos and once a patient has been diagnosed there are various potential sources of compensation available including trust funds, lawsuits, Veteran Administration claims, and sometimes workers compensation. It is best to meet with an experienced mesothelioma lawyer who can provide guidance on all of these. In fact, there are time limits (called statute of limitations) so it is best to meet with a lawyer sooner than later.
Pleural Mesothelioma Survival

There is a lot of depressing information on the internet about pleural mesothelioma and the survival associated with this cancer. Reading it, you would think that no one has ever survived this disease beyond a year or so. This information is far from comprehensive and can be misleading. To help balance the negative information that is so prevalent on the web, we present some case histories of long-term pleural mesothelioma survival, as published in the peer reviewed medical literature.
The medical literature are articles written by doctors and scientists for doctors and scientists. These pleural mesothelioma case histories are instructional in two ways:
- they remind us that, like Paul Kraus, there are long term survivors of this cancer;
- they allude to the importance that the immune system may play in mesothelioma.
Cases of Pleural Mesothelioma
12+ Years with Pleural Mesothelioma
In 1994, a 58 year old man complained of chest pain and shortness of breath. He had been exposed to asbestos previously through his work and was eventually diagnosed with malignant pleural mesothelioma. The patient decided not to have any active treatment at that time and continued with his life. Five years later he had an enlarging painless mass on his chest wall. A needle biopsy confirmed it was malignant. The patient had a left thoracotomy, multiple pleural biopsies, and chest wall resection. Pathology reconfirmed that the mass was malignant pleural mesothelioma. Seven years after the chest wall resection and 12 years after the initial diagnosis, the patient has no symptoms and no evidence of recurrence. No chemotherapy or radiation had been given.
The doctors who wrote up this case history for publication noted that there was “moderate host inflammatory response” and that “spontaneous regression may be an immune-mediated phenomenon.” In other words, the doctors hypothesized that the patient’s own immune system may have played a factor in his survival.
See: Pilling, J.E., et al., Prolonged Survival Due to Spontaneous Regression and Surgical Excision of Malignant Mesothelioma, Ann Thorac Surg, 2007; 83: 314-5.
14 Years of Pleural Mesothelioma
In 1986, a 65 year-old women had pain in her left chest wall. A chest X-ray revealed a small pleural effusion on this side. The patient declined an open biopsy and no diagnosis could be reached. She was treated for tuberculosis because of the high rate of this disease in her area. Her symptoms partially improved. In 1988 she had increasing pain over her chest. A biopsy was performed and malignant infiltration of the pleura was confirmed. She turned down treatment. In 1998, 10 years after the diagnosis of malignant pleural mesothelioma, she had an enlarging mass over her left chest wall. Biopsy confirmed the diagnosis of pleural mesothelioma. She had a course of radiation and died in January 2000, 14 years after her initial symptoms.
The doctors who wrote this report counseled their colleagues that long-term survivors can occur with pleural mesothelioma and “one should not hold the belief that it is always the intervention that prolongs survival.” In other words, these doctors suggested that in some cases the intervention (i.e. chemo, radiation, surgery) may not be the factor that prolongs survival in pleural mesothelioma, but other factors may be at work.
See: Wong, C.F., et al., A Case of Malignant Pleural Mesothelioma with Unexpectantly Long Survival without Active Treatment, Respiration March/April 2002; 69, 2: 166-168.
Over 7 Years with Malignant Pleural Mesothelioma
In 1970, a 53 year-old man had shortness of breath and a sharp pain on his right side. An X-ray revealed a right side pleural effusion. The patient had worked at a plant adjacent to the Brooklyn Navy Yard from 1955-1966 where asbestos had been used. In 1972 a thoracotomy was performed and a pleural biopsy was taken. The patient was diagnosed with malignant pleural mesothelioma. The patient never received any specific treatment for pleural mesothelioma. The report was written up in 1977 and apparently information about the continued life of this patient was not published after. We do not know how many more years or decades he lived.
The doctors noted in their discussion that, “This unusual course may be explained either by the presence of low-grade malignancy or by the unusual host resistance… Our findings are consistent with the concept that normal immunological function may effectively impede dissemination of the disease (malignant pleural mesothelioma).” In other words, these doctors are again alluding to how the immune system may play a role in managing pleural mesothelioma.
See: Fischbein, A,. et al., Unexpected Longevity of a Patient with malignant Pleural Mesothelioma, Cancer 1978; 42:1999-2004.
Spontaneous Regression of Malignant Pleural Mesothelioma
In 2015, an article was written by researchers at the Mayo Clinic and published in the Annals of the American Thoracic Society titled “Spontaneous Regression of Malignant Pleural Mesothelioma in a Patient with New-Onset Inflammatory Arthropathy.” In this article, they described how a case of mesothelioma regressed by itself after the patient experienced an inflammatory arthropathy. Inflammatory arthropathies are usually associated with increases in joint fluid, associated with increases in joint fluid
Infection and Spontaneous Regression
In an article about Spontaneous Regression of thoracic malignancies written by doctors at the Department of Medicine, North Shore University Hospital and Long Island Jewish Medical Center, the authors stated, “Infection may cause an immunologic reaction resulting in eventual fibrosis of the metastatic lesions.” In other words, an infection could trigger the immune system to help contain a metastatic thoracic cancer like mesothelioma.
See: Kumar, T., et al., Spontaneous regression of thoracic malignancies. Respir Med. 2010 Oct;104(10):1543-50.
Coley’s Toxins

This concept was first suggested by Dr. William B. Coley over a century ago:
In 1891, Coley injected streptococcal bacteria into a patient with inoperable cancer. He thought that the infection would have the side effect of shrinking the malignant tumor. He was successful, and this was one of the first examples of immunotherapy.
The Father of Immunotherapy
According to Dr. Edward F, McCarthy of the Department of Pathology and Orthopaedic Surgery, The Johns Hopkins Hospital:
“Over the next forty years, as head of the Bone Tumor Service at Memorial Hospital in New York, Coley injected more than 1000 cancer patients with bacteria or bacterial products. These products became known as Coley’s Toxins. He and other doctors who used them reported excellent results, especially in bone and soft-tissue sarcomas.
Despite his reported good results, Coley’s Toxins came under a great deal of criticism because many doctors did not believe his results. This criticism, along with the development of radiation therapy and chemotherapy, caused Coley’s Toxins to gradually disappear from use. However, the modern science of immunology has shown that Coley’s principles were correct and that some cancers are sensitive to an enhanced immune system. Because research is very active in this field, William B. Coley, a bone sarcoma surgeon, deserves the title ‘Father of Immunotherapy.'”
See: Edward F McCarthy, MD, The Toxins of William B. Coley and the Treatment of Bone and Soft-Tissue Sarcomas. Iowa Orthop J. 2006; 26: 154–158.