The Power of Immune Cells: Understanding Mesothelioma’s Microenvironment

In a recent study, researchers looked at how the body’s immune system responds to pleural mesothelioma, a type of lung cancer. The published their results in Pathobiology.
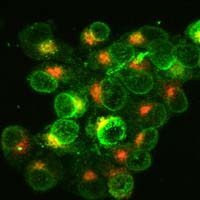
Researchers looked at samples from 60 pleural mesothelioma patients to study immune cells in the tumor area. They used markers to identify cell types and their impact on the disease. This study sheds light on using the immune system for improved treatments.
Immune Cells and Mesothelioma
Pleural mesothelioma is a type of cancer that affects the lining of the lungs. It is often caused by exposure to asbestos, a harmful mineral that was used in many industries in the past. Pleural mesothelioma is rare, but it can be very aggressive and difficult to treat.
A recent study looked at how the immune system responds to pleural mesothelioma. The immune system is the body’s defense against infections and diseases. It includes different types of cells. They can recognize and destroy harmful invaders, like bacteria, viruses, and cancer cells.
A Key to Better Treatment?
The study analyzed samples from 60 patients who were diagnosed with pleural mesothelioma. The researchers used a technique called immunohistochemistry. It studies markers on immune cells within tumors. The markers helped identify the type and job of immune cells. They were in the tumor microenvironment.
The researchers found that some immune cell markers were linked to a worse outcome. This was for patients with pleural mesothelioma. For example, high levels of CD3, CD4, CD8, CD163, and FOXP3+ immune cells were linked to worse outcomes. These cells regulate the immune response. Sometimes, they help cancer cells evade immune detection.
The study also looked at immune checkpoint receptors. These are proteins on immune cells that help regulate the immune response. They found that high levels of PD-1, CD27, and TIM-3 receptors on tumor-infiltrating lymphocytes were linked to worse survival. Immunotherapy drugs can target these receptors. They help the immune system fight cancer.
Researchers used hierarchical clustering analysis to group pleural mesothelioma samples by immune cell features. They found three groups. One had high immune cells, another had low, and a third had medium.
It was found that the group of pleural mesothelioma patients with high immune cell count had the worst survival rates. The study also identified specific proteins, such as CD47, CD70, and PD-L1, found in high levels in the tumor that can act as potential risk factors for these patients. These proteins have a role in regulating immune responses and can help cancer cells avoid detection by the immune system.
This study provides key insights. It shows the role of the immune system in pleural mesothelioma. It suggests that targeting certain immune cells and proteins in the tumor environment could be a promising approach. This could be a way to treat pleural mesothelioma in the future. More research is needed to confirm these findings and develop new treatments for this challenging disease.
Source:
Inaguma, Shingo, Chengbo Wang, Sunao Ito, Akane Ueki, Jerzy Lasota, Piotr Czapiewski, Renata Langfort, et al. “Characterization of Pleural Mesothelioma by Hierarchical Clustering Analyses Using Immune Cells within Tumor Microenvironment.” Pathobiology: Journal of Immunopathology, Molecular and Cellular Biology, March 25, 2024. https://doi.org/10.1159/000538520.